Clinical Experience: EMT
This is the first post in our series, highlighting various clinical experiences that high school and college students can participate in to prepare them for graduate school and careers in healthcare. The goal of this series is to help students learn not just the roles and responsibilities of common pre-health clinical experiences, but also to teach students how to obtain these positions. Feel free to reach out to me if you have any questions about my experience!
A few disclaimers:
EMT classes, scopes of practices, and other details about this article vary significantly depending on the county and state! This information is generally based on Michigan around the Ann Arbor area. I tried to make my statements general, but you should assume that any class details, local protocols, or basically anywhere is county and state-dependent.
This article will discuss some mature topics (death, overdoses, mental health etc.), which are unfortunately all regular parts of medicine.
Additionally, I would highly recommend watching this video made by one of my own personal mentors about University of Michigan’s Campus Ambulance service. It gives great insights into what being a student EMT is like: (https://www.youtube.com/watch?v=s_8Tas0bC7k)
What is an EMT?
EMT stands for Emergency Medical Technician. First of all, I want to make the distinction between paramedics and EMTs, as this is commonly misunderstood. There are 3 levels of being an EMT: basic, advanced, and paramedic (not including EMRs which are below EMTs). In this article, when I refer to “EMTs” I mean basic EMTs. I will discuss the differences between these levels later!
The most common place for EMTs to work is on an ambulance, but having an EMT license enables you to work in a variety of settings, including other clinical jobs like patient care techs, medical assistants, etc. (more on these positions in other posts).
What are EMTs trained to do?
EMTs are trained to identify life threatening conditions and provide critical treatments to stabilize patients for transport to the hospital. For example, EMTs are taught to assess the ABCs (airway, breathing, circulation) to find issues that can lead to serious issues before we can get the patient to the hospital. This can vary from county to county, but here are some skills that EMTs are licensed to perform:
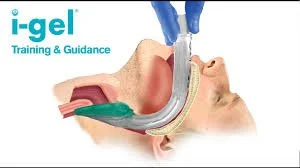
Supraglottic airway placement to help breathe for unconscious patients (see left)
Delivering a baby (and dealing with some of the basic complications that occur)
Basic medication administration (here are a few examples):
Aspirin for potential heart attacks to prevent further platelet aggregation
Ondansetron (Zofran) to treat nausea (pretty new skill for EMTs in some Michigan counties)
Albuterol to treat some conditions that involve difficulty breathing (Asthma, COPD, etc.)
Epinephrine for severe allergic reactions
Trauma injury stabilization (spinal stabilization, splinting, tourniquet)
Basic cardiopulmonary resuscitation (CPR) for cardiac arrest
How to become an EMT?
To become an EMT, you need to take a certification course (these are typically a few months long give or take based on the frequency of classes). Each class is different, but mine was over the course of one semester with classes lasting several hours on two nights per week.
These are commonly hosted by universities/community colleges, fire departments, and ambulance services. I took the class through Huron Valley Ambulance (which I would highly recommend if you live in the Ann Arbor area). In addition to the class, you have to obtain clinical hours involving “third-rides” (ride-alongs in an ambulance) and shadowing a nurse in the emergency room.
After the class, you have to pass a scenario based psychomotor test and the online NREMT test (a national EMT knowledge test). Lastly, after receiving your national license, you must become licensed at the state level (usually just some paperwork).
Differences between EMT licensure levels
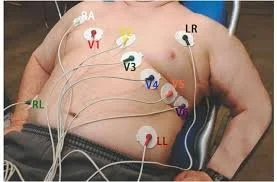
The scope of practice of basic EMTs are listed above. Paramedics have much larger scopes of practice, including reading EKGs (advanced cardiac monitoring), intravenous medication administration (and access to many other medications such as narcotics for pain relief), and advanced airway interventions (endotracheal tubes and cricothyrotomy [see below]). To become a paramedic, you must be a basic EMT first, take a 1-2 year class, and complete hundreds of clinical hours involving third rides and rotations through the hospital.
Advanced EMTs (AEMTs) are in between paramedics and basic EMTs.
Instructions for a cricothyrotomy: a last-resort procedure when other methods of obtaining an airway on an unconscious patient fail. This involves cutting into the patient’s neck to bypass the upper airway.
What do EMTs ACTUALLY do?
Here is the question that you are probably most interested in, what do EMTs actually do? A quick disclaimer: the unique thing about being an EMT is that you need to be ready to use any and every piece of equipment and knowledge that you learned in EMT school. Critical patients can require immediate interventions and you as an EMT need to be ready for anything in your scope of practice (i.e. no one will warn you ahead of time that you are going to be delivering a baby in the back of an ambulance).
Now that we have that out of the way, just like any other job, most of being an EMT is learning on the job and doesn’t exactly fit what you learn in school. First, let’s talk about the non-clinical parts of being an EMT. Here is a list of some maybe unexpected, but very common responsibilities that you have as an EMT:
Lifting patients out of sometimes very tight spaces (many patients cannot move themselves for a variety of reasons)
Wiping down equipment and “making” your stretcher after calls for the next patient
Driving long distances (again not every call is emergent)
Documenting literally everything that happens on a call
As you can see, being an EMT is (most of the time) like any other job! Most calls are routine and don’t involve much treatment. We will discuss what clinical responsibilities EMTs have in the next section.
Interfacility Transport vs. 911 Response
There are two main paths for EMTs to work on when working on an ambulance: interfacility transport and responding to 911 calls. Let’s define some terminology first:
Interfacility Transport (IFT): Transporting patients that can’t get themselves home or between facilities (e.g. they are bedbound or might be legally required to be transported by ambulance). These patients are VERY STABLE as they have already been evaluated by a medical team and are not expected to decline during transport (of course you must be ready for anything, but these patients rarely have issues).
Basic Life Support (BLS): Basic EMTs provide BLS care. This just means that your scope of practice doesn’t include more advanced interventions that are available to paramedics. Therefore, BLS ambulances (in the Ann Arbor area at least) frequently do not respond to 911 calls (unless resources are limited or the 911 call is clearly able to be handled by a BLS responder).
Advanced Life Support (ALS): Paramedics provide ALS care. This is the highest level of care typically offered for 911 calls. However, paramedic staffing can become extremely limited so BLS units are frequently utilized in many counties.
Ambulances can be classified by these designations above (e.g. there are plenty of ALS ambulances that do IFT when call volume is low). Where I work, we have BLS ambulances and ALS ambulances. BLS ambulances are typically responsible for any IFT duties and respond to 911 calls if ALS unit availability is limited. Again, this is all extremely dependent on where you work.
IFT Clinical Responsibilities
Since these patients are very stable, your clinical responsibilities are very minimal. Typically they just include taking basic vitals (heart rate, pulse oximetry, blood pressure, blood glucose, temperature) and ensuring that patients are not decompensating during transport. However, you get to practice talking to patients, taking vitals, and basic assessments so that when you respond to 911 calls, you are ready to perform these skills in the heat of the moment.
Frequently, these transports can be several hours long and are pretty uneventful. Keep in mind you have to drive back too!
911 Clinical Responsibilities
Every EMT will tell you that most calls are not critical, meaning patients don’t often require life saving treatment. Most of being an EMT is ruling out immediate life threats, which are few and far between, and transporting patients to the hospital.
Clinical responsibilities on a 911 call rely on your patient assessment. Some examples of assessments:
Is the patient’s airway patent? (e.g. are they choking, are they too unconscious to protect their own airway, etc.)
Is patient’s breathing effective? (e.g. are they breathing too shallow, are they breathing too fast or too slow)
Is the patient’s circulation effective? (e.g. is blood actually reaching tissues?)
Each of these assessments depends on your observation of clinical findings in patients. For example, if you want to know if someone has normal circulation, you can observe their skin color, temperature, capillary refill, etc.
Sample EMT Call
I am going to further illustrate the role of an EMT (and why being an EMT is sometimes hard) by walking through a sample call.
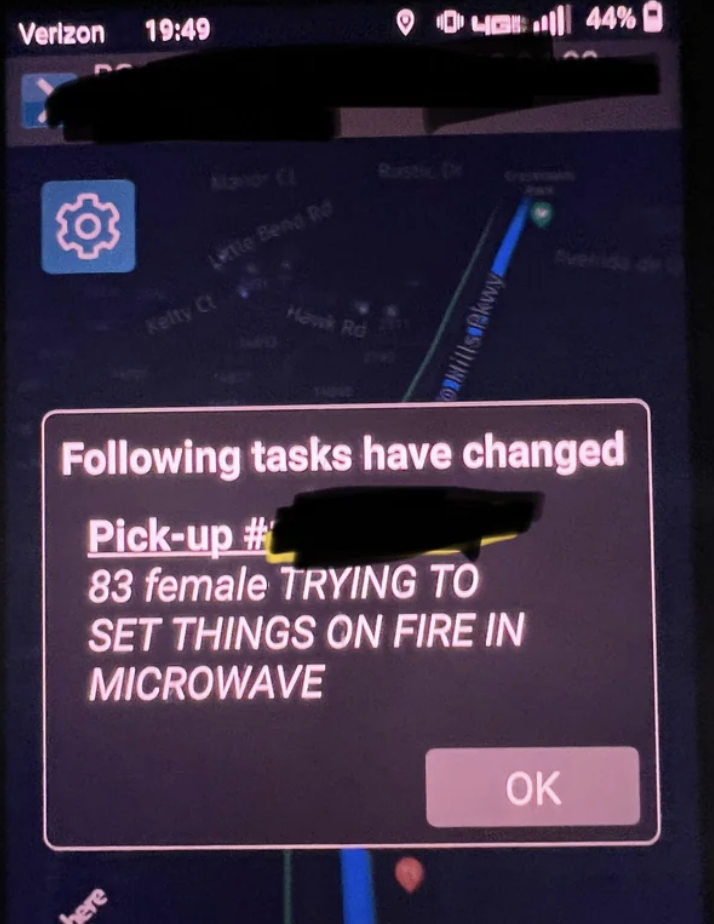
You are an EMT working on an ALS unit (with a paramedic who can provide ALS care). You are dispatched for an elderly woman who has fallen and can’t get up on her own. There are no apparent injuries. See right for some sample call notes that you might receive 🙂
First you have to drive to the scene! You turn on your lights and sirens and navigate through traffic, changing your siren pattern at every intersection, and eventually reverse your gigantic ambulance into someone’s small residential driveway (we always reverse into places for a quick exit).
You walk into the house and find an elderly woman on the ground not in any apparent distress and no blood is visible on the floor. Immediately, you don’t find any obvious life threats (her airway, breathing, and circulation seem to be intact). There’s two ways this call can go. Most of the time it is simple, you can help the woman to her feet and get her back in bed after reviewing the risks of not going to the hospital after she assures you that she is not injured. It can also be complicated…
When someone (especially at this age) falls we as EMTs want to know some important information (here are just a few of them):
Did you hit your head?
How did you fall?
Are you in any head/chest/neck/back pain?
What does your medical history look like/what medications do you take?
Are you acting normally?
We don’t ask these questions just to be nice, they are essential to understanding if you could be having a serious issue. For example, if you hit your head, you could be experiencing bleeding in your brain that you are unaware of. This head injury can also manifest as an altered level of consciousness (i.e. acting strangely or being unaware of your surroundings). We want to know what medications you take because if you take a blood thinning medication (which prevents your blood from clotting to stop bleeding), any small injury could turn bad and fast. Lastly, we want to know why you fell to make sure we aren’t missing a medical issue that CAUSED the fall. Falls can be due to mechanical issues, like tripping or losing your balance, or they can be due to a medical issue, like a cardiac issue which made you pass out. We are looking for any loss of consciousness/memory before/during your fall here.
Now, let’s assume you convince your patient to go to the hospital because they can’t remember how they fell and they aren’t acting right. You have to figure out how to get your patient from the floor to the hospital. Your patient fell while they were trying to stand up after using the bathroom and landed in between the toilet and the shower (this is often referred to as the Bermuda triangle of EMS… see a picture right). Imagine trying to maneuver a heavy patient out of this small area.
Your patient is overweight and is not able to get up on their own. You might use a tool like a patient mover (a glorified mat with handles - see below) to lift your patient off of the ground.
There are several issues here. Your patient is too heavy to be lifted by you and your partner alone. Now you need some help from firefighters (who you probably should have asked your dispatcher for as soon as you walked in the door because they are 10 minutes away). Your patient didn’t just happen to fall on this mat. How will you get it under them? This is going to involve rolling the patient from side to side if they are in a very tight area (and maintaining spinal stabilization as they could have a spinal injury from their fall).
You, your partner, and the firefighters pick this patient up and put them on your stretcher and load them into your ambulance. In the ambulance, you take basic vitals and attach this patient to the cardiac monitor. Although cardiac monitoring is not in your scope of practice, it is one of your paramedic partner’s roles, meaning you should know how to set it up for them (see below).
Now you drive this patient to the hospital (your partner sits in the back with this patient since they require cardiac monitoring which is above your pay grade). You don’t use lights and sirens now because your patient is stable enough where you aren’t worried about any immediate clinical issues (it is very common to not use lights and sirens to maintain the safety of you, your partner, and the patient during transport unless absolutely necessary).
Your partner gives a report to the hospital over the radio and to the nurse when you get to the hospital. You help slide the patient from the stretcher to the hospital bed. You clean the stretcher and your partner types a very long report detailing everything that just happened.
Now imagine if this patient had an actual cardiac issue, started losing consciousness during transport, or had a severe head injury. Also imagine that you are dispatched on a BLS unit to this call without access to cardiac monitoring. In this case, you would want to request an ALS unit if available!
Day in the life of an EMT
Every shift can look different. Shifts typically last between 6-24 hours. In between calls you can sit in a station or in your ambulance most likely in a parking lot. All of this is extremely variable.
Shifts start with checking your ambulance, making sure you have all of the possible equipment that you could need, testing electronics and communication devices, and setting up your ambulance for the day. Between the start and end of your shift, you can run calls all day or have free time all day (and anywhere in between). At the end of your shift, you restock the ambulance, wash the ambulance and its interior, and complete any remaining paperwork.
Career options after being an EMT
Being an EMT/Paramedic is extremely versatile. Here are some examples of careers that you can go into during/after getting an EMT or Paramedic license:
Critical Care Medicine → additional school to learn how to transfer critical patients from hospital to hospital on the ground or in a helicopter (think unstable patients that are in comas, taking high-risk medications, etc.)
Event Medicine → working at events to provide medical care to spectators and performers/athletes.
Community Medicine → caring for patients in their home to prevent them from returning to the hospital.
Healthcare Professions → you can go back to graduate school to become a nurse, physician assistant, doctor, etc.
EMT for medical school
For those of you who are interested in going to medical school, you probably know by now that you will need to get some sort of clinical experience. In my opinion, being an EMT is one of the best options out there! You get to interact with tons of different types of patients, clinical presentations, and fields of medicine.
Pros of being an EMT
There are a ton of pros to being an EMT! I have listed some off the top of my head:
Meaningful clinical contact with patients (you actually get to help them and save a life sometimes) and a wide variety of presentations
Exciting experiences for both medical and non-medical reasons (from helping resuscitate a patient in cardiac arrest to watching the roof of someone’s car get pried off by the fire department’s jaws of life to driving an ambulance through a drive-thru)
Depending on where you work, you can have a lot of downtime between calls. You can sleep, watch TV, do homework, etc. and if you get to sit in a station you might get a real bed!
You get to drive an ambulance…. (it is exactly as fun as it would seem)
Cons of being an EMT
Unfortunately, there are also cons to being an EMT. In my opinion, the pros 100% outweigh the cons and I love my job. However, I do want to acknowledge that there are real problems in EMS and the field of medicine as a whole. Here are a few that I think about:
Verbal/physical abuse from patients - one frequent cause of this is patients who don’t want to go to the hospital even though they have a real health concern but cannot make medical decisions for themselves (typically due to intoxication, injury that could cause altered mental status, or mental health concerns). Personally I haven’t had too many negative experiences with patients, but it does happen too frequently.
Burnout - EMS shifts are typically 12 hours or longer and “full-time” for many employees is much more than 40 hours/week. Additionally, 911 calls don’t stop at night or on holidays meaning you don’t either! For part-time students, this may be manageable, but it is hard for career EMTs with kids. Combine this with staffing shortages, low pay, and patients who call 911 for non-emergent issues and you burn out fast.
Expensive services - many patients will express their frustration with how much emergency care costs.
Conclusion
Overall, being an EMT is an awesome experience. EMS is by no means a perfect field, however, I think the pros far outweigh the cons in my experience. Personally, being an EMT has pushed me out of my comfort zone and made me significantly more comfortable talking to patients and dealing with high stress situations. I have learned so much about medicine as a field and the basic physiology and diseases that affect the human body. I have enjoyed working with different coworkers and healthcare professionals, learning about their backgrounds and gaining new clinical knowledge from each of them. I wouldn’t be applying to medical school without this experience and I would recommend it to any pre-med looking for clinical experience.
Feel free to reach out to me if you have any questions about my experience!
- Jacob Robins, EMT-B (jhrobins@umich.edu)